Can Spine Surgery be fully Automated?
A futuristic view informing today's decisions
What is not forbidden by the laws of nature, is possible given the right knowledge.
Problems are inevitable, problems are soluble.
David Deutsch, “The Beginning of Infinity”
Introduction
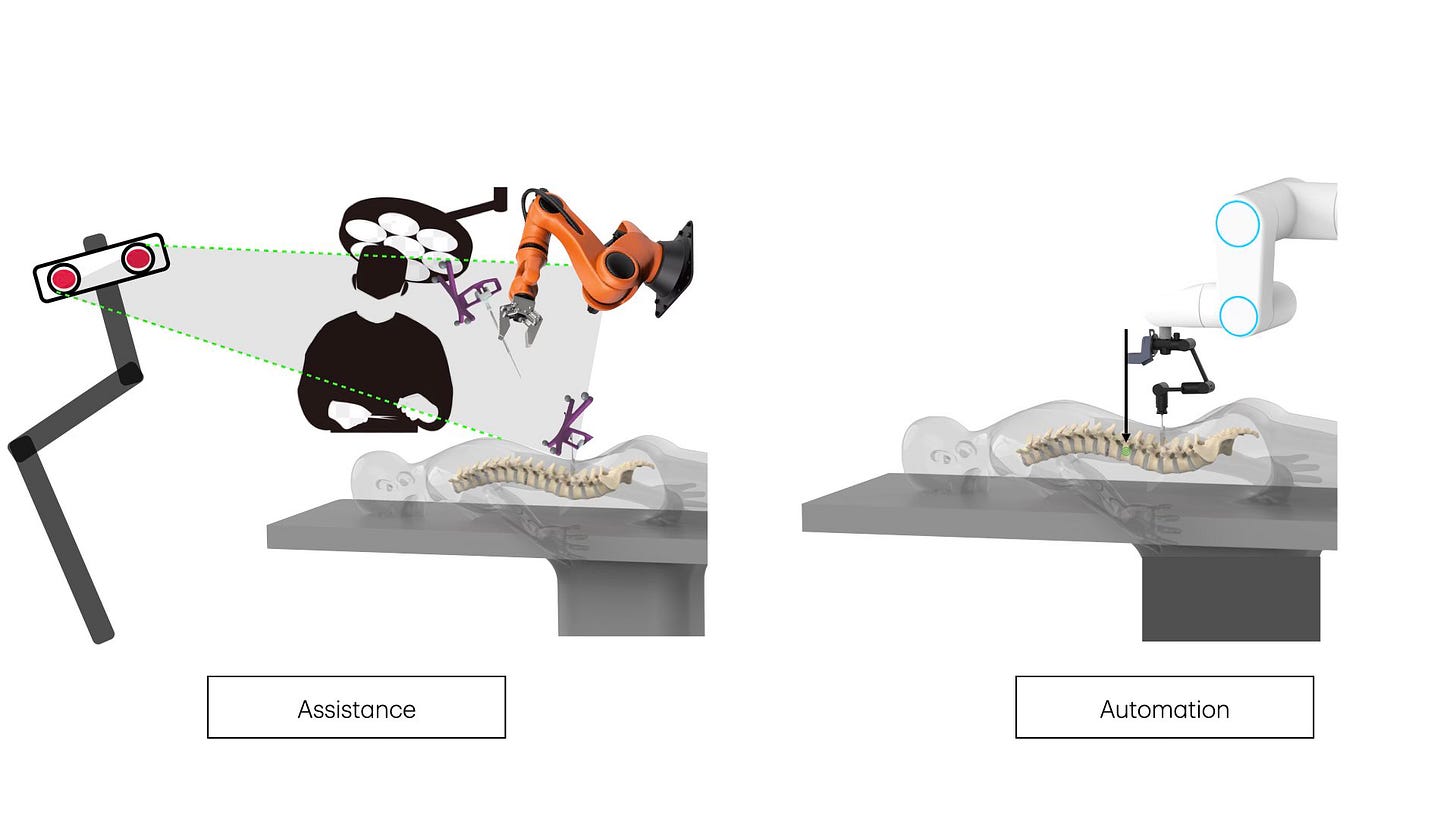
In this article we explore the possibility of fully automated spine surgery. These procedures would resemble today’s stereotactic radiosurgical operations in the sense that the rol of surgeons would be roughly limited to planning and supervision, while a machine (a robot of sorts) would fully executes the procedure. Our purpose is not to forecast the long term future. Our aim is rather to inform present day decisions regarding the allocation of time, passion, and other resources. Should we assist surgeons augmenting their capabilities with advanced tools? or, should we instead build a machine that takes over the procedure? To that aim, the current problem situation, the state of the art, and the challenges that the field spine surgery faces, are briefly reviewed and discussed with a pragmatic perspective.
A brief visit to a modern factory in the industrialised world (say, a cars factory), would make uncontroversial the idea that present day technology, particularly robotics, allows for full automation of spinal surgery. During the industrial process the ideas are precisely specified on blueprints, for example the special configuration and materials of a part of the engine. Those instructions are fed into the machine. A human operator provides the rough materials and supervises the process, the process is then repeated as many times as necessary. In such situations, what is automated is the less important non-creative repetitive task, the creative task remain in the brain of the car designer. What is not automated is the production of new ideas, the attempted solutions to problems, the design and the instruction contained in the blueprints.
The analogy is limited since people suffering from back problems are not cars in one specific sense; while cars of the same model intended to be all equal, there are not two patients alike. While the same blueprint can be used for as many cars as necessary, every single patient requieres their own specific plan. Every patient is unique. That is the reason why, given the current technology, surgeons remain essential. Although it might be consider that current artificial intelligence (AI) is capable of doing the planing by itself, we argue that that is not the case, that a whole solution to the patient health problem requires creative thinking. On the other hand, AI is being applied and will increasingly be used assisting planning.
Present day knowledge about spinal diseases and spinal mechanics is extensive, albeit incomplete. The specific relationship between structural changes caused by the diseases and the signs and symptoms are not fully understood. For example, it is possible to encounter significant structural aberrations in the spine without symptoms and the opposite. The challenge is that, while the objectives of the surgery are clinical (for example pain relief), the aim of the surgery is structural, decompression, stabilisation or deformity correction.
Perhaps the most relevant gap in our knowledge is in the field of chronic pain, which is by far the leading reason for spine surgery. Pain is a poorly understood brain function that is sometimes caused or triggered by spinal deformity, compression of the neural structures, instability, and degeneration. A significant advance in the knowledge of chronic pain, and the potential development of an effective and convenient treatments, would be highly disruptive to the field of spine surgery, as statins or endovascular treatments were for cardiac surgery. How many patients would demand spine surgery if pain is taken out of the equation?
Whether spine surgeons are aware or not, to address the challenges that every patient brings to the clinical practice, they use human ingenuity, guesswork, conjectures, and creativity. When available, AI tools assist the natural intelligence of the surgeons in planning procedures. However, current AI technology is not equipped to solve the type of problems found in spinal surgery which go far beyond the recognition of patterns.
The translation of the problem situation of the patient into the structural plan of the surgery will remain a human task at least until further breakthroughs in AI take place.
Spinal degeneration and gravity
Spine surgery is one of the most complex fields of human surgery. The chief reason for spine surgery is spinal degenerative disease, a process that largely overlaps normal aging. Degeneration of the spine might actually affect up to 100% of the humans living long enough. The number of surgical procedures have consistently increased over time, and the ceiling could potentially match that of the global aged population. On top of that, in a futuristic view, surgical procedures are not only used to mitigate the effects of diseases, they are also used to up-grade humans capabilities.
Degeneration of the spine is attributed to many factors, such as genetics, postural stress, physical activity, nutrition, metabolism, and age. This degeneration can be understood as the consequence of the action of gravity over the only bipedal species living on planet earth. Degeneration seems to stop when humans are deprived from gravity as experience with astronauts showed. (A futuristic treatment or rehabilitation strategy to spine structural problems might be to send patients to “gravity friendly” environments). Most of the time this process of degeneration is more or less silent, it does not produce specific or relevant signs and symptoms. But the degeneration of the spine in always manifest: it is the reason for the lost of heigh that comes with age, the increase in the forward curvature of the body, de impairment of balance, and the stiffness of the neck and torso.
The theory and the praxis
A theory that explain how the symptoms and signs are related to the structural alteration is implicit to every surgery, as well as an explanation of how these problems will be solved by the surgery. Most of the time, the theory appears to us as so simple that we take it for granted, but we shouldn’t. Only when theories are explicit they can be taken seriously, criticised, and improved. Here is an example of one of such theories: the collapse of the disk causes the adjacent vertebrae to come closer together, the foramina are reduced, the segmental movements altered, the exiting nerve roots compressed. The degeneration and altered biomechanics causes the back pain and the legs or tight pain is explained by root compression. A procedure that directly or indirectly decompress the roots and stabilises the spinal segment will eliminate the signs and symptoms.
The surgery itself is the crucial test for our implicit theory. Would the results be good, our theory is not disproven. However, more often than we wish, our theory is proven wrong by the persistence of sign and symptoms after surgery. In those cases we cannot be sure if (1) a less than perfect execution of the plan is to be blamed, or (2) rather the plan itself, the theory. The full automation of procedures could potentially rule out the former (1) reason for failure. In this sense, full automation is not only a way to improve the technical aspect of the surgery, importantly it might help us to improve our theories drastically reducing the effect of imprecisions and technical failure.
It is critical for the advance of the field to exercise an honest criticism of results, procedures, and their implicit theories. It is highly informative to know if a given suboptimal result was a problem of execution (the structural aims were not completely achieved) or it was the diagnosis and the plan the reason for failure.
Correcting the structure to fix the function
Spine surgery could be condensed to a limited set of mechanical or structural manoeuvres: (1) stabilisation, (2) bone removal, (3) ligaments, and intervertebral disk resection, (4) deformity correction (5) vertebral augmentation, and (6) joint reconstruction. The aim of this tasks is to correct the specific structural anomalies of the spine. By correcting the structure, it searches to eliminate pain, improve function, and the quality of life of patients.
1. Structural stabilisation
Structural instability is surgically addressed by vertebral fusion. In these procedures, two or more adjacent vertebrae are glue together with the intention of permanently block the movements between them.
Each vertebrae articulates with the one above and the one below through three joints: the intervertebral disk in front, and two paired zygapophyseal joints in the back. A successful fusion procedure must permanently eliminate movements in all three joints.
In the past, the fusion of adjacent vertebrae was achieved by removal of the cartilaginous part of the join and the addition of bone grafts. The following physiological process of bone growing and healing did the rest, building fresh bone bridges across the vertebrae. These procedures were highly invasive and required the patient to remain immobilised for long periods. It was soon recognised that the addition of stabilising hardware increased the rate of fusion and allowed faster recovery and immediate mobilisation.
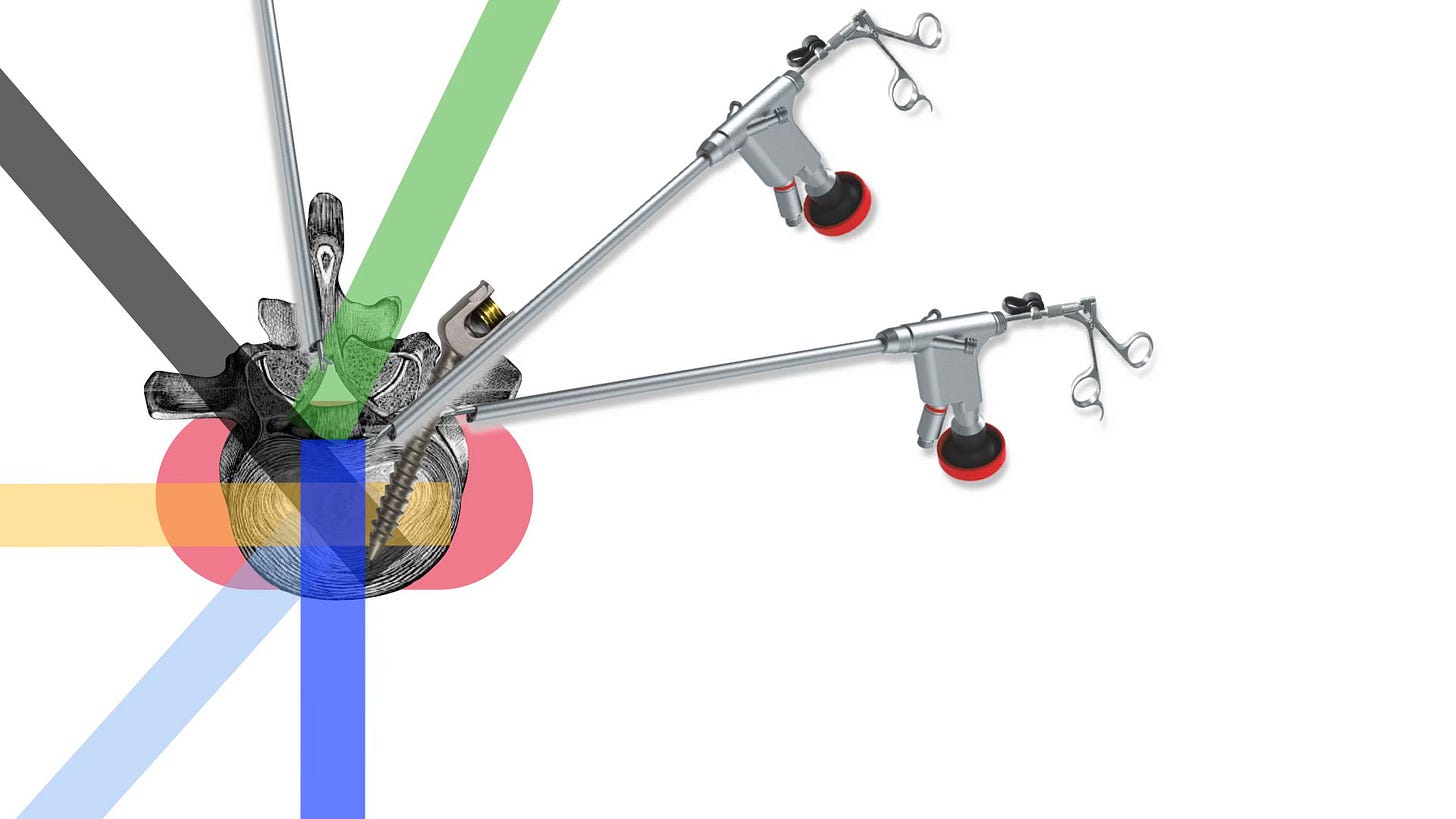
The introduction of pedicle screws in the seventies and eighties opened the way to less invasive and more reliable fusion procedures with no need of postoperative immobilisation. A whole new and prosperous industry of spinal implants had born. Since then, the indications for fusion and for spinal surgery largely increased and have never ceased to do so. The global market for spinal devices was valued in more that 11 billon USD in 2018 and it is projected to reach 16 billon in 2026.
Placing spinal implants such as pedicle screws is a complex surgical procedure with risk of serious complications. Besides the potential harm to the patients, the economic implications of the erroneous placement of these implant might be monumental. The world record for monetary compensation for medical malpractice in medicine is for a patients in whom pedicle screw misplacement resulted in paraplegia.
It takes several years to train a human to perform spine surgery. On top of the years of medical school, they should be trained as neurosurgeons or orthopaedic surgeons and then specialise in spine surgery. Considered together, the training of one of these surgeons takes around 14 years.
The technical suitability of pedicle screws placement couple with the increased demand for the procedure, the need to avoid complications, the financial incentives, and the long period of training competent spinal surgeons make the implementation of robotics difficult to resist. The avoidance of one single litigation case would be enough, at least in the US, to pay the bill of implementation.
2. Bone resection
The spine contains the spinal cord and the spinal nerves that connect the brain to the body. These neural structures are accompanied by blood vessels and are covered by the meningeal membranes. The degeneration process causes the spinal joints to overgrow, eventually compressing the neural structures. The most basic procedure in spine surgery is perhaps the laminectomy. Laminectomy consist in the resection of the posterior part of the vertebral arc (bone and ligaments) to decompress the spinal cord, the nerve roots, or both.
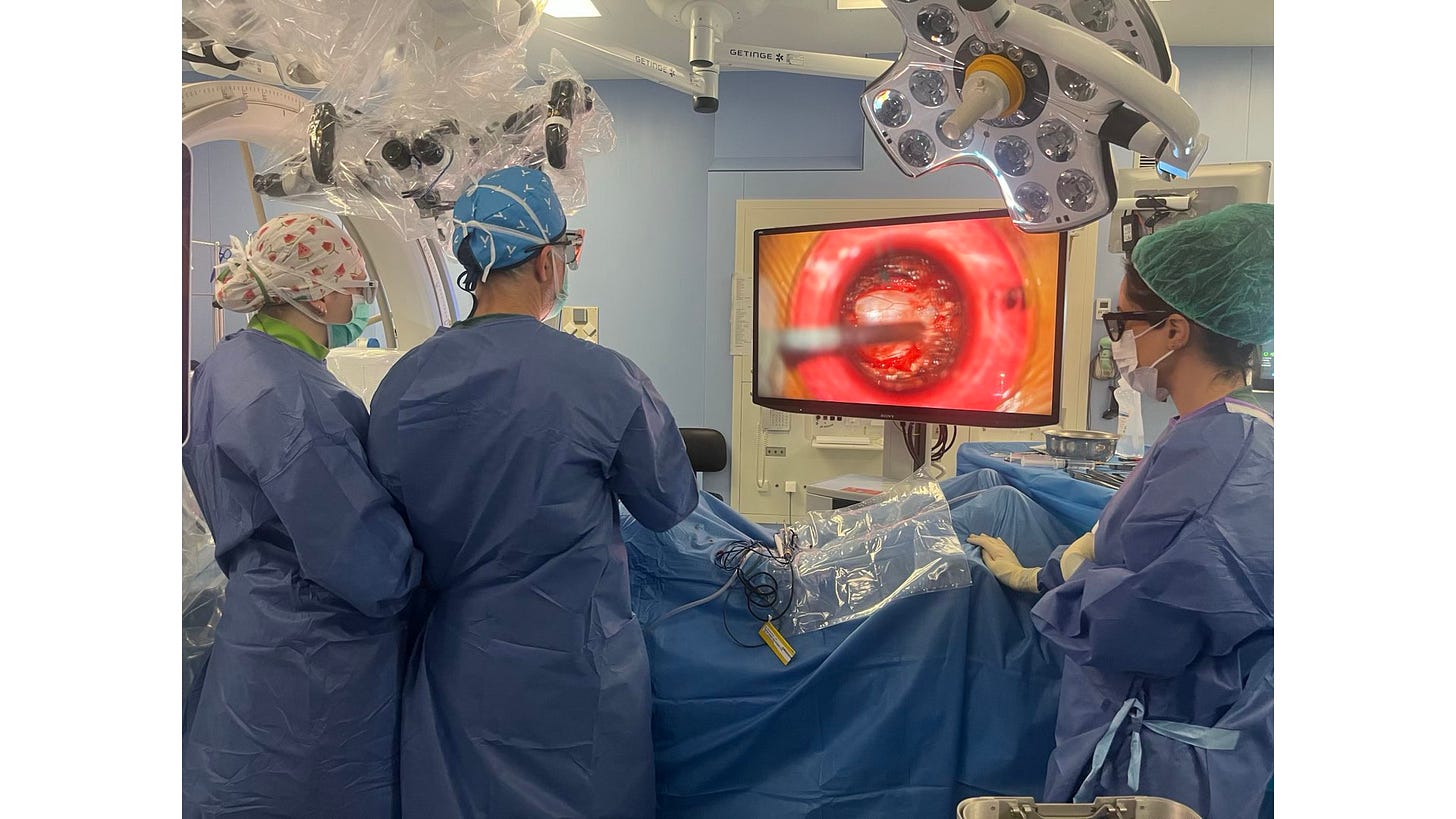
Laminectomy is classically performed exposing the spine from the back and removing bone in mechanical manner with the help of soft tissue retractors, suction, electrocautery, chisel, drills, and rongeurs.
In the last decades, bone removal was refined with the introduction of less invasive soft tissue retractors and high speed drill. Alternative, ultrasound based curettes, and laser devices were or are being developed with less success. The least invasive laminectomy is the so called “full endoscopic” technique. In these procedures, bony decompression is achieved percutaneously, without the need for soft tissue retraction.
The bone removal is currently performed under visual control. This control can be improve with loupes, surgical microscopes, or endoscopes. However, the achievement of a thorough decompression is difficult to confirm for several technical reasons and largely depends on the experience of the surgeon and the nature of the case. One obvious pitfall is the fact that the symptoms and sometimes the actual compression is only present is the standing position while the surgery is performed in ventral decubitus and the images that based the diagnosis in supine.
3. Intervertebral disk resection
The process of degeneration of the spine is often accompanied by disk colapse. The disk itself degenerates, losses height, and is often dislocated. As a consequence, the adjacent vertebral bodies approach each other and the intervertebral foramina are reduced compressing the nerve roots. The coronal and sagittal segmental curvature is also altered. Typically, the loss of the anterior height of the disk in the lumbar region causes hipo-lordosis. When the process of degeneration is asymmetric sidewise, it is manifest as coronal plane misbalance.
The surgical strategies to correct these structural anomalies range from sequestrectomy (removing only the dislocated part) the partial or near complete removal of the disk couple with the restoration (through inter-body implants) of the disk heigh and segmental lordosis. These structural objectives are usually achieved placing inter-body implants, artificial cages specially designed and adapted to the surgical approach. Currently, implants are designed primary to be adapted to the surgical approach rather than to the mechanical problem of the patient.
Given the complex biomechanics of the spinal joints, arthroplasty (joint replacement) is not widely used. Current technologies allows for the restoration of the structure of the spinal segment, height and curvature at the expense of its mobility. Additionally, the precision in achieving the planned structural objectives is low (i.e matching the planned lordosis), and complications in adults deformity surgery are reported in up to 40% of the cases.
The disk can be approached and removed percutaneously or with several open strategies from the front, the lateral, or the back of the spine. These procedures could potentially be automated and ad hoc implants designed to restore the structure and promote fusion. In this regard the innovation on expandable technology is relevant, these types of implants are expanded only when placed in the proper position. However, more innovation is needed to properly match the structural challenge. For example, the structure of the endplate is stronger around the perimeter and weaker toward the middle. Those implant with small contact surface and those placed towards the center are prone to subsidences especially in cases of osteopenia.
4. Deformity correction
Among the functions of the spine, one is to maintain bipedalism with the least expenditure of energy. However, to stand and walk using as little muscular contraction as posible is an extremely complex task. In physiological conditions this objetive is achieved through the development and maintenance of a complex curved structure -the spine- based upon the pelvis, and the associated ligaments and muscles, couple with a precise control of strength and coordination by de CNS.
Robert Playter, CEO of Boston Dynamics put the problem of locomotion in simple words when referring to the challenges of creating robots able to walk like humans. “The humanoid form [of robots] is attractive in many ways, but is also challenging. You have this big upper body that has a lot of mass and inertia. Throwing that inertia around increases the complexity of maintaining balance, and as soon as you pick something up with your arms, you make that problem even harder”. In other words, bipedalism is a complex task, and the structure of the spine is central to it. It is interesting to think that for robots, as for humans, the right alignment is that that is achieve with the least energy consumption. It took the evolution (countless iterations of variation and natural selection, i. e. trial and error) hundreds of thousands of years to achieve bipedalism and it did it without looking for it, it was a viable solution to the problems that our species needed to face. That is the reason why bipedal locomotion is so attractive, it solves in a very efficient way, the challenges of locomotion while freeing the hands and sight in the particular conditions of the surface of this planet.
The pelvis determines the shape of the spine and is determined by genetic and other factors. For the system to work properly, the curves of the spine (namely, cervical lordosis, thoracic cifosis, and lumbar lordosis) must be in accordance with the particular shape of the pelvis. Disruption of the normal curvatures of the spinal are associated with back pain, decreased functionality and poor quality of life.
Nowadays, the spine can be reshaped with surgical means. The procedure is highly complex and the results only match the planned shape within certain degree of error. In adults, the current rate of postoperative serious complication of this surgery was estimated to be about 40%. The procedures imply variable amounts of bone removal and vertebral fusion. One of the most effective procedure to correct fixed deformity is the pedicle subtraction osteotomy (PSO). The procedure consist in the removal of a wedge shaped piece of vertebra followed by fusion of at leat five vertebral segments. The osteotomy point serves as a hinge of the new created curve. In plain words, to correct adult deformity of the spine, first it needs to be cracked, then reshaped, and finally fused.
The technical challenges of automation
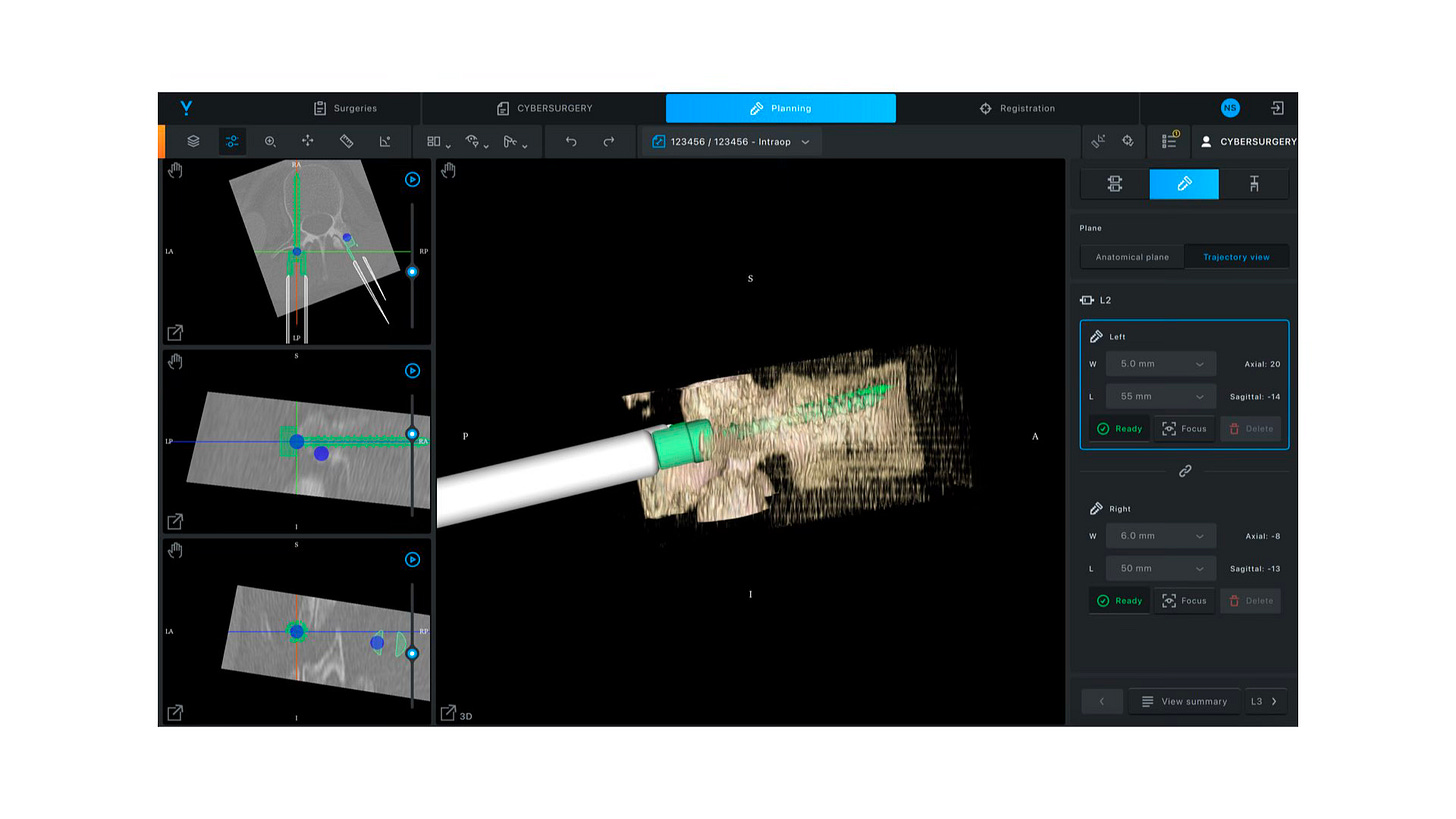
The automation of pedicle screws placement is the most obvious task to be trusted to robots. Not surprisingly, all robots currently available in spine surgery are (almost) exclusively used to establish trajectories that the human surgeon utilises to place pedicle screws. These machines are built over the optic navigation system that were intensively developed for cranial surgery and are based in an optic tracking system
While current navigation technologies and robotics are designed to assist surgeons, it could be argued that this fact is the main pitfalls for the current of innovation projects. The concept of designing an assisting machine (cobots, to be operated by a human) differs considerably from those used to design an autonomous robot (a machine that follows a plan). Paradoxically, it might also be technologically easier to design an autonomous robot than an assistant for humans.
Tracking the patient
Current robotic systems integrate navigation and are largely based on optic tracking. The technology is designed is such a way to show the surgeon the structures hidden from their vision. However, several limitation of the optical tracking system might limit the ability to build automation further over it. Among those limitations, the necessity of clear area for the cameras to track the fiducial, the distance of the camera to the objective, and the necessity to compute images; might considerably affect real time tracking and precision.
A new tracking system seems crucial in order to facilitate the automation of pedicle placement and specially other tasks that need more precision, opening the way to automatic robotic bone and disk resection, and deformity correction.
Bone resection
Robotic drilling of the bone is the next step of clinical application. Currently, the most efficient and precise way to remove bone is mechanical drilling (milling in the industrial terminology). Ultrasound and laser based technology are other possibilities.
The challenge is to design the best way to introduce and drive the bone removal toll to the spine and to guide it with enough precision. One posible solution is the use of soft tissue dilators and tubular retractor such as those used in minimally invasive surgery (MIS). Another interesting option is to access the spine percutaneously as it is performed in the full endoscopic procedures. Additionally, the system can be dispensed with optical systems, since the robot does not necessary need visual control during drilling.
Automation of disk removal and inter body implants
Disk removal and interbody implants such as TLIF cages can be automatised. This task will require the design of specific tools adapted to the physical properties of the disk as well as implants.
Automation of deformity correction
Segmental and global deformity correction can be automatised through AI algorithms and robotics. Some current system are already advanced in that sense. Robotic could potentially add precision, reliability and speed-up the procedure. For example, with advanced automatic robotic drilling, percutaneous and fast PSO might become a reality, potentially drastically increasing the safety of the procedure.
Problems derived from automation and criticism
Automation may expand rather than eliminate the field of possible problems as compared to the human surgeon. Those would certainly arise, but they might be also new and better problems. Every solution worthy of its name comes with improvements and problems and they are impossible to predict. For that reason, it is important to remain critical toward every proposed innovation; precaution is good. Conversely, the “precautionary principle” (do not innovate if something wrong could potentially happen) equals to the prohibition of innovation and progress.
Automation allows for standardisation, removing the operator’s variability from the equation. Standardisation will allow the growth of knowledge of the physiopathology of the human spine, as a result of the elimination of variability in the procedures. This would increase or capacity to test our best explanation and theory of sign and symptoms. One of such hypothesis could be as follow: for the decompression of spinal stenosis, it is sufficient to remove all the compressing element around the yellow ligament, leaving the ligament untouched. Automation of the bone removal will allow to test such hypothesis since it will increase pre precision of the bony removal in a reliable and reproducible manner.
The classic aim of automation is to replace human manual control, planning and problem solving by automatic devices and computers. The surgeon may be expected to monitor that the automatic system is operating correctly, and if it is not, they may be expected to call a more experienced operator or to take-over themself. But physical skills deteriorate when they are not used or trained, particularly the refinements of gain and timing. When manual take-over is needed there is likely to be something wrong with the process, so that unusual actions will be needed to deal with it, and one can argue that the operator needs to be more rather than less skilled, and less rather than more experienced, than average. Those and others are the new types of problem that we will need to face, and there is most to came since progress is unbounded.
Final words
There is no single thing in spinal surgery that cannot be improved. Although the future is unknowable, we have to make decision in the present only with insufficient information. Our decisions are made upon guesses, mere hypothesis about how to better solve a given specific challenge. Progress is both possible and desirable, and innovation is a moral obligation of every surgeon. Spinal robotics has a brilliant present and could benefit embracing the philosophy of “replacing the surgeon” instead of “assisting the surgeon” . However, achieving the last situation means to walk a number steps in which the surgeons’ hands and brain are still fundamental.
References
Virk S, Qureshi S, Sandhu H. History of Spinal Fusion: Where We Came from and Where We Are Going. HSS J. 2020 Jul;16(2):137-142. doi: 10.1007/s11420-020-09747-7. Epub 2020 Feb 25. PMID: 32523481; PMCID: PMC7253552.
Lisanne Bainbridge. Ironies of automation. Automatica Volume 19, Issue 6, November 1983, Pages 775-779.
Fritzell P, Hägg O, Nordwall A; Swedish Lumbar Spine Study Group. Complications in lumbar fusion surgery for chronic low back pain: comparison of three surgical techniques used in a prospective randomized study. A report from the Swedish Lumbar Spine Study Group. Eur Spine J. 2003 Apr;12(2):178-89. doi: 10.1007/s00586-002-0493-8. Epub 2003 Feb 14. PMID: 12709856; PMCID: PMC3784840.
Sankey EW, Mehta VA, Wang TY, Than TT, Goodwin CR, Karikari IO, Shaffrey CI, Abd-El-Barr MM, Than KD. The medicolegal impact of misplaced pedicle and lateral mass screws on spine surgery in the United States. Neurosurg Focus. 2020 Nov;49(5):E20. doi: 10.3171/2020.8.FOCUS20600. PMID: 33130620.
Here you can find further information about Cyber Surgery project: https://cyber-surgery.com
